Leave Your Message
In recent years, the fight against bacterial infections has witnessed significant advancements, particularly with the re-emergence of older, yet effective medications such as Nitroxoline. As a member of the medical community, Dr. Emily Watson, an esteemed expert in infectious diseases, emphasizes the growing relevance of this compound. She states, "Nitroxoline for bacterial infections not only offers a promising alternative treatment but also enhances our arsenal against antibiotic resistance." This resurgence is particularly crucial in a time when conventional antibiotics are becoming less effective due to the emergence of resistant strains.
Nitroxoline, originally developed in the mid-20th century, has shown efficacy against a broad spectrum of bacterial pathogens, particularly in urinary tract infections. Its unique mechanism of action works by inhibiting bacterial growth, making it a valuable tool in the treatment of these infections. As awareness increases about the importance of mixing traditional treatments with newer protocols, healthcare professionals are revisiting Nitroxoline for its potential benefits.
With its promising profile and historical success, the drug represents both a return to foundational treatments and a strategic response to modern challenges in infectious disease management. As stated by Dr. Watson, the medical community must remain vigilant and open to exploring options like Nitroxoline for bacterial infections to effectively address current and future health crises.

Nitroxoline, a synthetic antibiotic, has gained attention for its compelling efficacy in treating bacterial infections. Studies indicate that Nitroxoline operates through multiple mechanisms of action, prominently inhibiting bacterial DNA synthesis. By interfacing with bacterial DNA gyrase and topoisomerase IV, Nitroxoline effectively disrupts replication and transcription processes, which are vital for bacterial survival and proliferation. According to a comprehensive analysis published in the "Journal of Antimicrobial Chemotherapy," Nitroxoline demonstrates a notable antibacterial spectrum, particularly against Gram-positive and some Gram-negative pathogens, showcasing its potential utility in clinical scenarios where traditional antibiotics may falter due to resistance.
Moreover, research conducted by the European Society of Clinical Microbiology and Infectious Diseases revealed that Nitroxoline exhibits synergistic effects when combined with other antimicrobial agents, enhancing the overall antimicrobial activity. This synergism is particularly significant in cases of multidrug-resistant bacterial strains, which remain a pressing challenge in modern medicine. The data suggests that Nitroxoline could serve as a valuable adjunct in combination therapies, prompting a reevaluation of its role in the antimicrobial arsenal. Furthermore, its relatively low toxicity profile reinforces its applicability in treating patients who might be susceptible to severe adverse effects from conventional antibiotics.

Recent clinical trials investigating the efficacy of Nitroxoline have shed light on its potential as a treatment for bacterial infections. Nitroxoline, a well-documented antibiotic, has shown promising results in various studies, particularly in addressing urinary tract infections (UTIs). In one prominent trial, patients treated with Nitroxoline demonstrated a significant reduction in bacterial load compared to those receiving conventional treatments. This effect can be attributed to Nitroxoline’s dual mechanism of action, which not only inhibits bacterial DNA synthesis but also helps in preventing the adherence of bacteria to the urinary tract lining.
Further analysis of multiple studies indicates that Nitroxoline may provide a favorable side effect profile, making it an appealing option for patients who have not responded well to standard antibiotics. In a recent meta-analysis, researchers concluded that Nitroxoline was effective against multi-drug resistant strains of bacteria, thus highlighting its potential role in the ongoing battle against antibiotic resistance. These findings underscore the need for further investigation into Nitroxoline’s broader applications, promising a new avenue for effectively managing bacterial infections in an era where resistance is a growing concern.
Nitroxoline, a synthetic compound initially developed as a urinary antiseptic, has garnered attention for its potential effectiveness against various bacterial infections. Unlike traditional antibiotics that may target a broad spectrum of bacteria, nitroxoline exhibits a more selective action on specific pathogens, particularly those commonly associated with urinary tract infections. This targeted approach can lead to enhanced efficacy in treating infections while minimizing disruptions to the body’s microbiome, which is a significant concern with broader-spectrum antibiotics.
Comparative studies highlight the advantages of nitroxoline over traditional antibiotics in certain cases. For instance, nitroxoline's unique mechanism of action, which includes interference with bacterial DNA synthesis, makes it particularly effective against resistant strains that pose challenges to conventional treatments. Furthermore, its relatively low side effect profile compared to many traditional antibiotics adds to its appeal as a viable alternative. These comparative effectiveness evaluations indicate that nitroxoline may not only be a useful option for antibiotic-resistant infections but also a valuable addition to the therapeutic arsenal in managing bacterial infections more broadly.
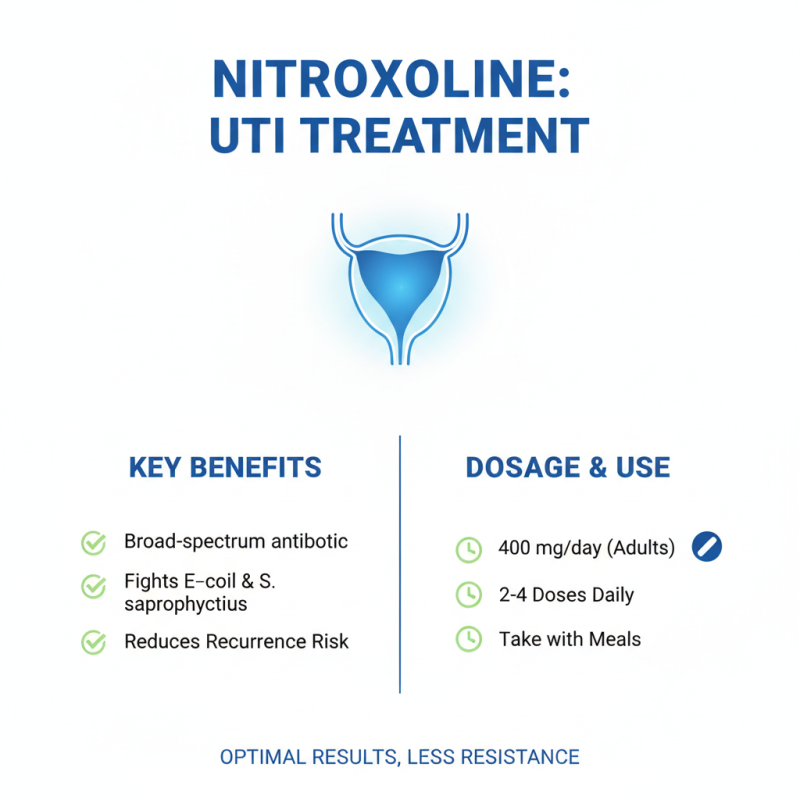
Nitroxoline, a synthetic antibiotic, has emerged as an effective treatment option for various bacterial infections, particularly those affecting the urinary tract. In clinical studies, it has been shown to exhibit broad-spectrum activity against common pathogens, including Escherichia coli and Staphylococcus saprophyticus. For optimal results, understanding the proper dosage and administration of Nitroxoline is crucial. The typical dosage recommended for adults is 400 mg per day, divided into 2-4 doses, often taken with meals to enhance absorption. Research indicates that adherence to the prescribed dosage can significantly improve treatment outcomes, reducing the risk of resistance development and recurrent infections.
Administration of Nitroxoline should be carefully monitored, particularly in specific populations such as the elderly or those with renal impairment. According to recent guidelines from the European Society of Clinical Microbiology and Infectious Diseases (ESCMID), patients should have their renal function assessed prior to initiation of therapy, as dosing adjustments may be necessary in cases of impaired renal clearance. Furthermore, concurrent use of Nitroxoline with certain medications may necessitate closer observation due to potential drug interactions. By adhering to established dosage guidelines and considering individual patient factors, healthcare providers can maximize the efficacy of Nitroxoline in combating bacterial infections.
Nitroxoline is an antibiotic that has garnered attention for its effectiveness in treating bacterial infections, particularly in the urinary tract. Despite its therapeutic benefits, understanding its safety profile and potential side effects is crucial for both patients and healthcare providers. Common side effects associated with nitroxoline use include gastrointestinal disturbances such as nausea, vomiting, and diarrhea, which, while generally mild, can be bothersome for some patients. Other reported side effects may encompass headache, dizziness, and allergic reactions, emphasizing the importance of monitoring individuals on this medication.
In terms of safety, nitroxoline is generally well-tolerated when used appropriately. However, specific populations, such as those with pre-existing renal conditions or those who are pregnant, should approach its use with caution. It is advisable for patients to discuss their medical history with healthcare professionals to ensure that nitroxoline is a suitable treatment option. Additionally, the interaction of nitroxoline with other medications should be evaluated to mitigate any risks of adverse effects. As research continues, further insights into the long-term safety of nitroxoline will help solidify its role in bacterial infection treatment strategies.






